WHAT ARE HEMORRHOIDS?
It is important to note that all people have hemorrhoidal tissue as part of their normal anatomy. Only in a minority of people do hemorrhoids become enlarged or otherwise symptomatic. Hemorrhoidal tissue lies within the anal canal and perianal area and consists of blood vessels, connective tissue, and a small amount of muscle.
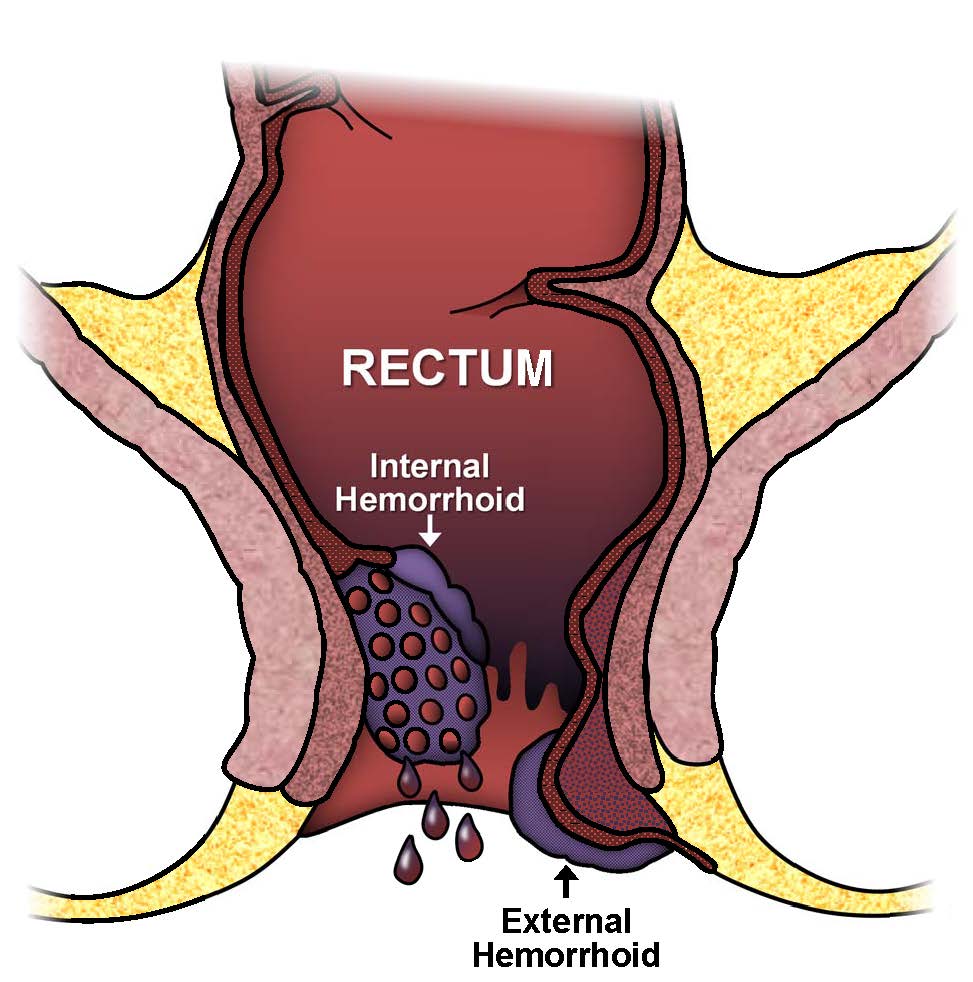
There are two main types of hemorrhoids: internal and external. Internal hemorrhoids are covered with a lining called mucosa that is not sensitive to touch, pain, stretch, or temperature, while external hemorrhoids are covered by skin that is very sensitive. When problems develop, these two types of hemorrhoids can have very different symptoms and treatments.
SYMPTOMS
Roughly 5% of people will develop symptoms attributable to their hemorrhoids and only a small fraction of those patients will require surgical treatment. Patients may experience symptoms caused by either internal or external hemorrhoids or both.
The majority of patients with anal symptoms seen in a colon and rectal surgeon’s office complain of hemorrhoids but a careful history and examination by an experienced physician is necessary to make a correct diagnosis. Some patients will have long-standing complaints that are not attributable to hemorrhoidal disease. Other serious diseases such as anal and colorectal cancer should be ruled out by a consultation with Colorectal provider who is knowledgeable in evaluating the anal and rectal area.
INTERNAL HEMORRHOIDS
Painless rectal bleeding or prolapse of anal tissue is often associated with symptomatic internal hemorrhoids. Prolapse is hemorrhoidal tissue coming from the inside that can often be felt on the outside of the anus when wiping or having a bowel movement. This tissue often goes back inside spontaneously or can be pushed back internally by the patient. The symptoms tend to progress slowly over a long time and are often intermittent.
Internal hemorrhoids are classified by their degree of prolapse, which helps determine management:
Grade One: No prolapse
Grade Two: Prolapse that goes back in on its own
Grade Three: Prolapse that must be pushed back in by the patient
Grade Four: Prolapse that cannot be pushed back in by the patient (often very painful)
Bleeding attributed to internal hemorrhoids is usually bright red and can be quite brisk. It may be found on the toilet paper, dripping into the toilet bowl, or streaked on the stool itself. Not all patients with symptomatic internal hemorrhoids will have significant bleeding. Instead, prolapse may be the main or only symptom. Prolapsing tissue may result in significant irritation and itching around the anus. Patients may also complain of mucus discharge, difficulty with cleaning themselves after a stool, or a sense that their stool is “stuck” at the anus with BMs. Patients without significant symptoms from internal hemorrhoids do not require treatment based on their presence alone.
EXTERNAL HEMORRHOIDS
Symptomatic external hemorrhoids often present as a bluish-colored painful lump just outside the anus. They tend to occur spontaneously and may have been preceded by an unusual amount of straining. The skin overlying the outside of the anus is usually firmly attached to the underlying tissues. If a blood clot or thrombosis develops in this tightly held area, the pressure goes up rapidly in these tissues often causing pain. The pain is usually constant and can be severe. Occasionally the elevated pressure in the thrombosed external hemorrhoid results in breakdown of the overlying skin and the clotted blood begins leaking out. Patients may also complain of intermittent swelling, pressure and discomfort, related to external hemorrhoids which are not thrombosed.
ANAL SKIN TAGS
Patients often complain of painless, soft tissue felt on the outside of the anus. These can be the residual effect of a previous problem with an external hemorrhoid. The blood clot stretches out the overlying skin and the skin remains stretched out after the blood clot is absorbed by the body, thereby leaving a skin tag. Other times, patients will have skin tags without an obvious preceding event. Skin tags will occasionally bother patients by interfering with their ability to clean the anus following a stool, while others just don’t like the way they look. Usually, nothing is done to treat them beyond reassurance. However, surgical removal is occasionally considered.
WHAT CAUSES SYMPTOMATIC HEMORRHOIDS?
The majority of factors thought to produce symptomatic hemorrhoids are associated with an increased pressure within the abdomen that gets transmitted to the anal region. Some of these factors include: straining when having a bowel movement, constipation, diarrhea, pregnancy, and irregular bowel patterns. It seems that, over time, these factors may contribute to the prolapse of internal hemorrhoidal tissue or enlargement of or thrombosis of external hemorrhoidal tissue.
EXAMINATION
After obtaining a careful history regarding your symptoms and your personal and family medical history, your doctor will need to perform an examination in the office. This usually consists of careful inspection of the outside of the anus, placement of a finger through the anus into the rectum (digital examination), and placement of a finger-sized instrument through the anus to allow visual inspection of the hemorrhoidal tissue (anoscopy). Although it may not occur during the initial visit, your doctor may want to look even further upstream into the colon to rule out polyps, cancers, and other causes of bleeding. A flexible sigmoidoscopy can visualize approximately half of your colon, while a colonoscopy usually allows for visualization of the entire colon.
NON-SURGICAL TREATMENT OF INTERNAL HEMORRHOIDS
There are a wide variety of treatment options available for symptomatic internal hemorrhoids depending upon their grade (see above discussion) and the severity of your symptoms. Often, adherence to the dietary and lifestyle changes detailed below will relieve symptoms. However, if there is failure to respond to these changes alone, or if symptoms are severe enough at the outset, there are a number of office-based and surgical procedures available to alleviate symptoms.
DIETARY/LIFESTYLE CHANGES
The cornerstone of therapy, regardless of whether surgery is needed or not, is dietary and lifestyle change. The main changes consist of increasing dietary fiber, taking a fiber supplement, getting plenty of fluids by mouth, and exercising. This is all designed to regulate, not necessarily soften, your bowel movements. The goal is to avoid both very hard stools and diarrhea, while achieving a soft, bulky, easily cleaned type of stool. This type of stool seems to be the best kind to prevent anal problems of almost all kinds.
It is usually recommended to achieve 20-35 grams of fiber per day in the diet, including plenty of fruits and vegetables. Most people can benefit from taking a fiber supplement one to two times daily. These supplements are available in powder, chewable, and capsule/tablet forms. Also important is adequate fluid (preferably water) consumption, often considered 8-10 glasses daily. Caffeinated drinks and alcohol tend to be dehydrating and therefore do not count toward this total.
OFFICE-BASED THERAPIES FOR INTERNAL HEMORRHOIDS
The most commonly used office procedures are rubber band ligation, infrared coagulation, and sclerotherapy. These treatment options are for internal hemorrhoids only and do not apply to external hemorrhoids.
RUBBER BAND LIGATION
Rubber band ligation can be used for Grades 1, 2, and some Grade 3 internal hemorrhoids. At the time the MD or APP performs the examination described above (anoscopy), a device can be placed through the anoscope, which can pull up the excessive internal hemorrhoidal tissue and place a rubber band at its base. The band acts to cut off the hemorrhoid’s blood supply and the extra tissue falls off (with the band) at roughly 5-7 days, at which time there may be a small amount of bleeding. If a patient is taking blood thinners such as Coumadin, Heparin, or Plavix, they may not be a candidate for this procedure. Anywhere from one to three rubber bands per visit may be placed and several short visits may be required to achieve relief of symptoms. Rubber band placement is not associated with any significant recovery time for most people. Rubber bands can be associated with a dull ache or feeling of pressure lasting 1-3 days that is usually well-treated with Ibuprofen or Tylenol. Upon completion of your banding session(s), you likely will not need further treatment, provided you continue the previously described dietary and lifestyle changes. If your symptoms return, repeat banding certainly can be considered. Hemorrhoidectomy is always an option if significant progress is not made with banding. Complications are very uncommon, but may include bleeding, pain and infection, among others.
INFRARED PHOTOCOAGULATION
Infrared coagulation (IRC) is another office-base procedure, for Grades 1 and 2 and occasional Grade 3 internal hemorrhoids, which can be performed during anoscopy. IRC utilizes infrared radiation generated by a small light that is applied to the hemorrhoidal tissue. This energy is converted to heat and causes the hemorrhoidal tissue to become inflamed, slough off, and scar down, thereby eliminating this excess tissue. This procedure is usually quick, painless, has few complications, but may take several short sessions to achieve relief of symptoms.
SCLEROTHERAPY
Sclerotherapy is another office-based treatment for Grades 1 and 2 internal hemorrhoids. It involves the injection of chemical irritants into the hemorrhoids, resulting in scarring and shrinkage by reducing the blood vessels present in the hemorrhoidal tissues. Sclerotherapy is similarly quick, often painless, has few complications, and may take several short sessions to achieve relief of symptoms. This has the potential to be used in patients taking blood thinners such as Coumadin, Heparin, or Plavix, but would need to be considered.
OFFICE TREATMENT OF EXTERNAL HEMORRHOIDS
External hemorrhoids, which are not thrombosed, are generally managed symptomatically, with dietary management and topical agents. Only occasionally are they removed surgically but this cannot be done in the office.
The pain associated with a symptomatic, thrombosed external hemorrhoid (see description above) often peaks about 48-72 hours after its onset and is largely resolving after roughly four-five days. Pain is the indication to treat thrombosed external hemorrhoids and, therefore, the treatment will depend upon the timing from the initial thrombosis. If you are improving significantly and your doctor is able to touch/pinch the involved external hemorrhoid without significant discomfort to you, then non-operative measures are used (warm baths, pain-relieving creams and pills, and fiber therapy described above). If a patient presents in severe pain, an office-based surgical procedure may be offered. This involves the injection of local anesthesia (“numbing medicine”) and removing the blood clot and overlying skin.
OPERATIVE TREATMENT OF HEMORRHOIDS
Fewer than 10% of all patients evaluated with symptomatic hemorrhoids will require surgical management. Most patients respond to non-operative treatment and do not require a surgical procedure. Hemorrhoidectomy, or surgical removal of the hemorrhoidal tissue, may be considered if a patient presents with symptomatic large external hemorrhoids, combined internal and external hemorrhoids, and/or grade 3-4 prolapse. Hemorrhoidectomy is highly effective in achieving relief of symptoms and it is uncommon to have any significant recurrence. However, it also causes much more pain and disability than office procedures and has somewhat more complications.
Hemorrhoidectomy may be done using a variety of different techniques and instruments to remove the hemorrhoids and the particular technique is usually chosen based on a particular surgeon’s preference. In basic terms, the excess hemorrhoidal tissue is removed and the resultant wound may be closed or left open. Hemorrhoidectomy is performed in an operating room and may be done under sedation, general anesthesia, or under a spinal block (similar to an epidural injection during childbirth).
In an attempt to avoid some of the postoperative pain associated with hemorrhoidectomy, a stapled or suture hemorrhoidopexy may be considered and involves pulling the hemorrhoids upward, returning the problematic hemorrhoidal tissue to its normal position. All operative procedures for hemorrhoidal disease carry their own set of risks and benefits and the ultimate choice of procedure must be made between you and your surgeon.
POSTOPERATIVE INSTRUCTIONS
Pain can be expected following hemorrhoid surgery. The goal is to make it manageable, but it may be up to 2-4 weeks before one is able to resume your full level of activities. Pain medication is usually a combination of narcotic and non-narcotic medicine and the goal is to limit the amount and number of days a patient takes stronger narcotic medications. Sitting in a bath (sitz bath) 2–3 times daily for 10-15 minutes per time in warm water can be quite helpful. Occasionally, patients will have difficulty urinating after anorectal surgery. If unable to void, the patient should try urinating in the tub during a sitz bath. If that does not work, a patient should be instructed to contact the Surgeon’s office and/or proceed to an emergency department for placement of a catheter in the bladder. Failure to do so can result in permanent bladder damage from over-stretching.
Bowel movements after hemorrhoid surgery is a concern for patients. Most colon and rectal surgeons recommend having a stool within the first 48 hours after surgery. A high fiber diet, a fiber supplement, and increased liquid intake are advised. If this does not produce a stool, laxatives may be indicated. Occasionally, a second procedure has to be done under anesthesia to remove (disimpact) the stool.
WHAT IS A COLON AND RECTAL SURGEON?
Colon and rectal surgeons are experts in the surgical and non-surgical treatment of diseases of the colon, rectum and anus. They have completed advanced surgical training in the treatment of these diseases as well as full general surgical training. Board-certified colon and rectal surgeons complete residencies in general surgery and colon and rectal surgery, and pass intensive examinations conducted by the American Board of Surgery and the American Board of Colon and Rectal Surgery. They are well-versed in the treatment of both benign and malignant diseases of the colon, rectum and anus and are able to perform routine screening examinations and surgically treat conditions if indicated to do so.
DISCLAIMER
The American Society of Colon and Rectal Surgeons is dedicated to ensuring high-quality patient care by advancing the science, prevention and management of disorders and diseases of the colon, rectum and anus. These brochures are inclusive but not prescriptive. Their purpose is to provide information on diseases and processes, rather than dictate a specific form of treatment. They are intended for the use of all practitioners, health care workers and patients who desire information about the management of the conditions addressed. It should be recognized that these brochures should not be deemed inclusive of all proper methods of care or exclusive of methods of care reasonably directed to obtain the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances presented by the individual patient.