Irritable bowel syndrome (IBS) is a common disorder affecting over 15 percent of the population. The following information has been prepared to help patients and their families understand IBS, including the symptoms, causes, evaluation, and treatment options.
IBS is one of a range of conditions known as functional gastrointestinal disorders. While no structural abnormalities exist and nothing abnormal is seen on tests, the bowel may function abnormally. IBS is sometimes referred to as spastic colon, spastic colitis, mucous colitis or nervous stomach . These are outdated terms. IBS should not be confused with Inflammatory Bowel Disease (commonly referred to as IBD) which is primarily made up of ulcerative colitis and Crohn’s disease. Importantly, treatment for IBS is medical, and surgery is not indicated for this problem.
WHAT ARE THE SYMPTOMS OF IBS?
People with IBS may experience abdominal pain and changes in bowel habits, either diarrhea, constipation, or both at different times. Patients often have symptoms that tend to be more diarrhea-predominant or constipation-predominant. Symptoms may be mild or severe and vary from person to person. The symptoms may come and go and can change over time. The most common symptoms of IBS are abdominal pain, fullness, gas and bloating. Other symptoms associated with IBS include abdominal cramps, generalized abdominal aches, abnormal stool consistency, and passage of mucous, urgency or a feeling of incomplete bowel movements. Symptoms often occur when there is a change in the frequency of bowel movements. IBS discomfort is often improved after a bowel movement.
WHAT CAUSES IBS?
While there is no definite cause of this syndrome, the symptoms of IBS seem to occur as a result of abnormal functioning or communication between the nervous system and the muscles of the bowel. This abnormal regulation may cause the bowel to be “irritated” or more sensitive. The muscles in the bowel wall may contract too forcefully or too weakly, or even too slowly or rapidly at certain times. Although there is no physical obstruction to stool, a patient may feel the cramps as if there were a blockage to the passage of stool through the colon.
IBS happens nearly twice more often in women than men. Sometimes IBS occurs after an intestinal infection — known as post-infectious IBS. Environmental factors, genetic factors, bacterial fermentation in the gut, bacterial overgrowth, food intolerance, altered bowel motility, intestinal hypersensitivity, altered nervous system processing, and alterations in hormonal regulation have all been considered as possible causes of IBS.
Recent studies suggest that IBS symptoms are not all caused by a single mechanism, but are the result of different mechanisms acting on the intestines. Intestinal irritants, such as poorly digested carbohydrates or fats, excess bile, intolerance of certain foods and genetic predisposition to intestinal inflammation may all play a role in the symptoms of IBS. These various factors in the intestines or bowel wall may activate reflexes that change intestinal function or secretion. Irritants may also stimulate nerves in the bowel wall leading to intestinal hypersensitivity and pain.
WHAT ROLE DOES STRESS PLAY IN IBS?
IBS is not caused by stress. It is not a psychological or psychiatric disorder; however, emotional stress may contribute to IBS symptoms. Many people may experience increased symptoms of IBS when nervous or anxious. Reducing the sources of stress in our lives may help to alleviate the symptoms of IBS.
HOW CAN I TELL IF THE PROBLEM IS IBS OR SOMETHING ELSE?
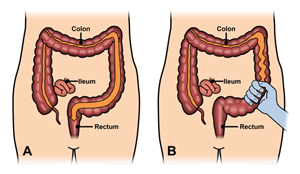
No test can confirm the diagnosis of IBS. Instead, it is often considered a “diagnosis of exclusion”, meaning other diseases must be ruled out before calling the problem IBS in a given patient. However, there are specific features that are needed to make the diagnosis of IBS, including abdominal pain or discomfort at least 3 days per month in the previous 3 months with two or more of the following features: improvement of symptoms after a bowel movement, onset associated with a change in frequency of stool and/or change in the form (appearance) of stool. A careful history and physical examination by a gastroenterologist, colon and rectal surgeon or other physician are needed to exclude more serious disorders. Tests may include blood tests, stool tests, flexible sigmoidoscopy or colonoscopy, and x-ray studies.
Fever, anemia (low red blood cell levels), rectal bleeding and unexplained weight loss are not symptoms of IBS and must be promptly evaluated by your physician. Other signs or symptoms that call for special consideration include: new onset of symptoms at age 50 or older, nighttime symptoms that awaken the patient, changes in symptom quality, recent use of antibiotics or family history of other intestinal diseases such as inflammatory bowel disease or cancer.
Eating a lactose-free diet for 2 weeks may help your physician check for a possible lactose intolerance that can cause similar symptoms.
HOW IS IBS TREATED?
Understanding that IBS is not a serious or life threatening condition may help relieve anxiety and stress, which contribute to the problem. Stress reduction, use of behavioral therapy, physical therapy, biofeedback, relaxation or pain management techniques can help relieve the symptoms of IBS in some individuals. Use of a diary may help identify certain foods or other factors that cause symptoms. Surgery is not indicated for IBS.
The goal of treatment is to relieve symptoms. Lifestyle changes such as regular exercise and improved sleep habits may be helpful. Dietary changes can also be helpful in some patients. Several different types of food substances seem to contribute to symptoms in patients with IBS. These foods are often referred to by the acronym FODMAP (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) and include complex sugars such as lactose, fructose, galactose, sorbitol, mannitol and xylitol. A low FODMAP diet may be beneficial in some people with IBS. Gluten intolerance may also contribute to symptoms in patients with IBS, even if they do not have celiac disease. Gas producing foods such as beans, cabbage, cauliflower, broccoli, brussel sprouts and onions may contribute to bloating and discomfort in people with IBS.
Dietary fiber can play either a positive or negative role in IBS. Soluble fiber such as that found in citrus fruits, flaxseeds and legumes may help soften stool and lessen the severity of cramps. Insoluble fiber found in cellulose, cereals and bran can absorb water and lessen diarrhea. In some people, too much fiber can increase bloating and cause discomfort.
Probiotics or “good bacteria” may also improve the symptoms of IBS and can be used to supplement other dietary changes. Probiotics come in different forms and it may take some trial and error to find one that works best for you.
Individuals with moderate to severe IBS may benefit from prescribed medication. No one medication will work for everyone. Medications that your doctor might try include: anticholinergic medications to help control intestinal spasms, such as dicyclomine, propantheline, belladonna, or hyoscyamine. Side effects may include dry mouth, difficulty urinating, blurred vision and racing heart beat. Bisacodyl can be used to treat constipation. Loperamide may be used to treat diarrhea. Antidepressants in low doses have been shown to be helpful in some with IBS. Rifaximin, an antibiotic used for 2 weeks, has been shown to be helpful in some patients without constipation who have IBS. This suggests that intestinal bacteria may play a role in causing IBS in some people.
HOW LONG DOES THE TREATMENT TAKE TO RELIEVE SYMPTOMS?
Relief of IBS symptoms is often a slow process. It may take six months or more for definite improvement to be appreciated. Patience is very important in dealing with this problem. The tendency for the intestine to respond to stress will always be present. With attention to proper diet and in some cases, use of appropriate medications, the symptoms of IBS can be greatly improved or eliminated.
WHAT IF I CHOOSE TO DO NOTHING?
IBS does not lead to more serious problems, and it does not cause cancer, bleeding or inflammatory bowel diseases such as ulcerative colitis. If nothing is done, symptoms will usually continue. The symptoms may come and go, they may get better or worse with time and may continue to impact your quality of life.
QUESTIONS FOR YOUR DOCTOR:
- What is IBS?
- What causes IBS?
- Does stress cause IBS?
- How is IBS diagnosed?
- Are there tests to confirm IBS?
- Do I need a colonoscopy or more tests?
- Is IBS a “serious illness”?
- Can IBS lead to other serious diseases?
- What are my options for treating IBS?
- Do certain foods affect my symptoms?
- Will my IBS symptoms resolve?
WHAT IS A COLON AND RECTAL SURGEON?
Colon and rectal surgeons are experts in the surgical and non-surgical treatment of diseases of the colon, rectum, and anus. They have completed advanced surgical training in the treatment of these diseases, as well as full general surgical training. Board-certified colon and rectal surgeons complete residencies in general surgery and colon and rectal surgery, and pass intensive examinations conducted by the American Board of Surgery and the American Board of Colon and Rectal Surgery. They are well versed in the treatment of both benign and malignant diseases of the colon, rectum and anus and are able to perform routine screening examinations and surgically treat conditions, if indicated to do so.
DISCLAIMER
The American Society of Colon and Rectal Surgeons is dedicated to ensuring high-quality patient care by advancing the science, prevention and management of disorders and diseases of the colon, rectum and anus. These brochures are inclusive but not prescriptive. Their purpose is to provide information on diseases and processes, rather than dictate a specific form of treatment. They are intended for the use of all practitioners, health care workers and patients who desire information about the management of the conditions addressed. It should be recognized that these brochures should not be deemed inclusive of all proper methods of care or exclusive of methods of care reasonably directed to obtain the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances presented by the individual patient.
SUGGESTED READINGS AND WEBSITES
Pub Med Health. Fact Sheet: Irritable Bowel Syndrome.
www.aboutibs.org/site/about-iffgd/
www.mayoclinic.com/health/irritable-bowel-syndrome/D5000106
CITATIONS
Foxx-Orenstein, A. IBS: Review and What’s New. Med. Gen. Med. 2006: 8-20
Nikfar, S., et.al.: Efficacy of Probiotics as a Treatment in Irritable Bowel Syndrome: A Meta-Analysis of Randomized Controlled Trials. Dis. Col. Rectum; 51(12): Dec.2008; 1775-1780
Talley, N.: Dietary Modification as a Treatment for Irritable Bowel Syndrome. Gast. Hep.; Aug. 2012; 552-554
Pimentel, M., Lembia, A., Chevy, W.D., et. al.: Rifaxamin Therapy for Patients with Irritable Bowel Syndrome Without Constipation. N Engl J Med; 2011; 364: 22-32
Camilleri, M.: Peripheral Mechanisms in Irritable Bowel Syndrome. N Engl J Med 2012; 367: 1626-1635
Madhulika G. Varma and Brooke H. Gurland, Chapter 32,”Constipation and Functional Bowel Disorders”. Chapter in Beck, D. E., Roberts, P. L., Saclarides, T. J., Senagore, A. J., Stamos, M. J., Wexner, S. D., ASCRS Textbook of Colon and Rectal Surgery, 2nd Edition. Springer, New York, NY; 2011.