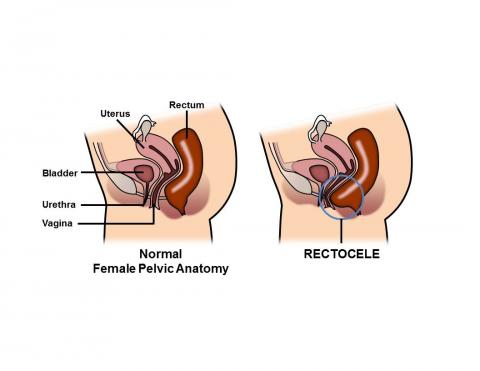
WHAT IS A RECTOCELE?
A rectocele is a herniation (bulge) of the front wall of the rectum into the back wall of the vagina. The tissue between the rectum and the vagina is known as the rectovaginal septum and this structure can become thin and weak over time, resulting in a rectocele. When rectoceles are small, most women have no symptoms. A rectocele may be an isolated finding or occur as part of a generalized weakening of the pelvic floor muscles. Other pelvic organs such as the bladder (cystocele) and the small intestine (enterocele), can bulge into the vagina, leading to similar symptoms as rectocele.
WHAT CAUSES A RECTOCELE?
The exact cause of a rectocele is unknown, but symptomatic rectoceles usually occur in conjunction with weakening of the pelvic floor. There are many things which can lead to weakening of the pelvic floor, including advanced age, multiple vaginal deliveries and birthing trauma during vaginal delivery (e.g. forceps delivery, vacuum delivery, tearing with a vaginal delivery, and episiotomy during vaginal delivery). In addition, a history of chronic constipation and excessive straining with bowel movements are thought to play a contributory role in developing a rectocele. Multiple gynecological or rectal surgeries can also lead to weakening of the pelvic floor and rectocele formation.
WHAT ARE THE SYMPTOMS ASSOCIATED WITH A RECTOCELE?
As previously noted, the majority of patients with a rectocele have no symptoms. In fact, approximately 40% of all women will have a rectocele found on routine physical examination. When symptoms are present, they may be categorized as either rectal or vaginal. Rectal symptoms may include: difficulty with evacuation during a bowel movement and the need to press against the back wall of the vagina and/or space between the rectum and the vagina (perineal body) in order to have a bowel movement. Vaginal symptoms can include the sensation of a bulge or fullness in the vagina, tissue protruding out of the vagina, discomfort with sexual intercourse, and vaginal bleeding.
Symptomatic rectoceles can lead to excessive straining with bowel movements, the urge to have multiple bowel movements throughout the day, and rectal discomfort. Fecal incontinence or smearing may occur as small pieces of stool can be retained in a rectocele (stool trapping), only to later seep out of the anus. Significant stool trapping can also result in an increase in the sense of needing to have a bowel movement, as the stool stuck in the rectocele returns to the low rectum when the patient stands, thereby giving the patient the urge to defecate again.
HOW CAN A RECTOCELE BE DIAGNOSED?
Examination of the pelvic region typically includes both a vaginal and rectal examination. This often includes a bimanual or speculum examination. Additionally, a digital rectal exam will be performed which usually demonstrates a weakness in the anterior wall of the rectum (the side closest to the vagina). A special x-ray, called defecography, can also visualize and confirm a rectocele. During this exam, the patient will sit and be asked to defecate on a specially-designed commode after contrast material is instilled in the rectum, vagina and bladder. If a rectocele is present, this study can document the size and the ability to completely empty the rectum. In general, if the rectocele is larger than 2 centimeters and/or has significant retention of contrast, it is considered abnormal.
HOW CAN A RECTOCELE BE TREATED?
A rectocele should only be treated if you are having significant symptoms that interfere with your quality of life. Prior to any treatment, there should be a thorough evaluation by your doctor. There are both medical and surgical treatment options for rectoceles. The majority of symptoms associated with a rectocele can be resolved with medical management; however, treatment depends on the severity of symptoms. Surgical treatment is reserved for only the most severe cases of symptomatic rectocele.
NON-SURGICAL TREATMENT OF RECTOCELE
The vast majority of a patient’s symptoms associated with a rectocele can be managed effectively without surgery. It is very important to have a good bowel regimen in order to avoid constipation and straining with bowel movements. A high fiber diet of 25+ grams per day can help with this goal. This may be achieved with a fiber supplement, high fiber cereal, or high fiber bars. Additionally, an individual should also increase her water intake, with 6-8 ten-ounce glasses daily. The combination of fiber and water will allow for softer, bulkier stools that do not require significant straining with bowel movements, thereby reducing your risk for having a symptomatic rectocele. Stool softeners are also recommended on occasion. During bowel movements, it is important to avoid straining, therefore, if you do not have the urge to have a bowel movement, do not force defecation. In addition, it is always important to avoid prolonged sitting periods on the toilet.
Biofeedback refers to exercises one performs with a provider to strengthen and retrain the pelvic floor and can also lessen the symptoms of a rectocele.
SURGICAL TREATMENT OPTIONS
The surgical management of rectoceles should only be performed if you continue to have symptoms despite the use of conservative measures such as fiber, water, and pelvic floor strengthening. These symptoms should be significant enough that they interfere with your activities of daily living, meaning that you cannot comfortably do the things you usually do on a daily basis. Colorectal surgeons, gynecologists and urogynecologists are trained in the diagnosis and treatment of this condition. These trained physicians can perform surgeries to attempt repair of a rectocele.
There are multiple ways to approach the surgery including: transanally (through the anus), through the perineum (the space between the anus and vagina), and through the vagina. All of these aim to remove the extra tissue that makes up the rectocele and reinforce the rectovaginal septum (the tissue between the rectum and the vagina). This can be done by plication (stitching the tissue together). Occasionally, mesh (a prosthetic material or patch) can be used to reinforce the repair.
The S.T.A.R.R. technique uses a special stapling device that removes the redundant tissue and staples it together at the same time. This technique should only be used if a patient has other problems such as obstructive defecation or mucosal prolapse (rectal tissue that protrudes out of the anus).
A rectocele can also be repaired through the abdomen, either laparoscopically or open. This approach has been proven safe and effective, but there may not be any benefit over other types of rectocele repair. The approach will depend on the size of the rectocele and the symptoms associated with the rectocele.
OUTCOMES OF SURGICAL REPAIR
The overall success of the surgery depends on the symptoms, length of time symptoms have been present, and approach of surgery. As with any surgical procedure, there are associated risks including bleeding, infection, new onset dyspareunia (pain during intercourse), fecal incontinence, rectovaginal fistula (a communication between the rectum and vagina), as well as a risk that the rectocele may recur or worsen.
Some studies report significant improvement in about 75-90% of patients. However, the success rates seem to decrease over time and, at two years, only 50-60% of patients can expect to have significant improvement. In addition, patients with fecal incontinence may have better results with a transperineal or vaginal approach, as the transanal approach has been shown to occasionally worsen continence. A surgeon who is familiar with the technique and has experience repairing rectoceles will have the best results.
WHAT IS A COLON AND RECTAL SURGEON?
Colon and rectal surgeons are experts in the surgical and non-surgical treatment of diseases of the colon, rectum, and anus. They have completed advanced surgical training in the treatment of these diseases, as well as full general surgical training. They are well-versed in the treatment of both benign and malignant diseases of the colon, rectum and anus and are able to perform routine screening examinations and surgically treat conditions if indicated to do so.
DISCLAIMER
The American Society of Colon and Rectal Surgeons is dedicated to ensuring high-quality patient care by advancing the science, prevention and management of disorders and diseases of the colon, rectum and anus. These brochures are inclusive but not prescriptive. Their purpose is to provide information on diseases and processes, rather than dictate a specific form of treatment. They are intended for the use of all practitioners, health care workers and patients who desire information about the management of the conditions addressed. It should be recognized that these brochures should not be deemed inclusive of all proper methods of care or exclusive of methods of care reasonably directed to obtain the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances presented by the individual patient.