OVERVIEW
An ostomy is a surgically created opening between an internal organ and the body surface. Ostomies are often created as a part of intestinal surgery when there must be a new way for intestinal waste to leave the body. This information was prepared to help patients understand what an ostomy is, learn how to live with an ostomy, relieve concerns they may have and assure them that they can enjoy an active and fulfilling life with an ostomy.
Patients and caregivers who are facing surgeries that involve an ostomy often have a number of questions:
-
How does an ostomy impact bowel movements?
-
Where will the ostomy be placed?
-
How will an ostomy affect the activities of my daily living, for example, my diet, clothing and bathing, work, physical activities, travel, and sexual intimacy?
-
Will other people know that I have an ostomy?
-
What are potential complications of an ostomy?
WHAT IS AN OSTOMY?
An ostomy is a surgically created opening between an internal organ and the surface of the abdominal wall. A circular incision is made in the abdominal wall and a piece of intestine is brought through the incision to lie partially outside the body wall. The part of the bowel that is seen on the abdomen surface is called a stoma. Ostomies may be used by the surgeon to treat complicated abdominal problems or to allow for healing of the site of surgery. Cancer, trauma, inflammatory bowel disease (IBD), bowel obstruction, infection, fecal incontinence (inability to control bowel movements), constipation, and diverticulitis (inflammation of tiny pockets that commonly form in the colon wall) are all possible examples of situations where surgery may involve an ostomy.
An ostomy is further identified by the part of the intestine involved. For example, an "ileostomy" is a surgically created opening involving the ileum, a part of the small intestine, to the skin of the abdominal wall. A "colostomy" is a surgically created opening involving a part of the colon, or large intestine, to the skin of the abdominal wall.
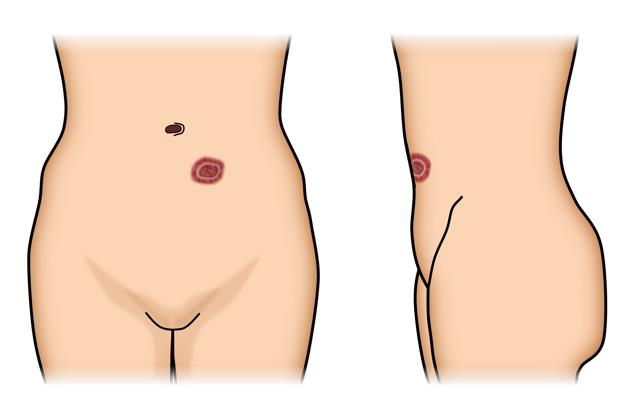
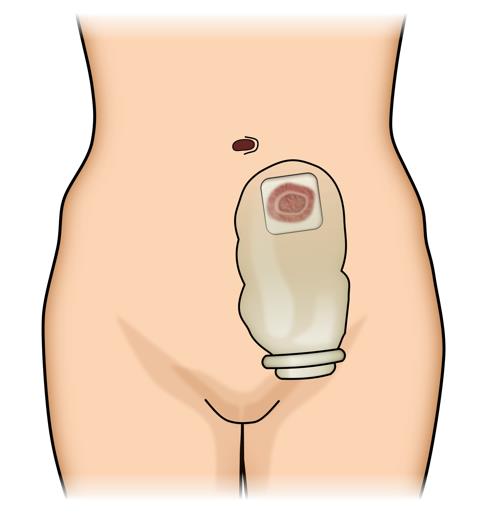
Figure 1: Ostomy and ostomy appliance (www.fascrs.org)
An ostomy may be temporary or permanent. A temporary ostomy is usually created in the process of treating complicated abdominal problems, or to divert the stool away and allow time for healing. A temporary ostomy keeps stool material away from a downstream area (towards the rectum or anus), such as a healing surgery site, an area of inflammation, or a blockage associated with disease or scar. Temporary ostomies may be reversed when considered appropriate by your colorectal surgeon. A permanent ostomy serves as a means for long-term stool evacuation. Instances of needing a permanent ostomy include when disease, or its treatment, impairs normal intestinal function, or when the anus or the muscles that control elimination must be removed or no longer work properly.
An ostomy may be constructed as an end ostomy or a loop ostomy, depending on the specific circumstances for which an ostomy is being created. An end ostomy is formed by bringing the end of a segment of bowel through the skin opening, and rolling the bowel’s end back onto itself, like a shirt cuff, and suturing the bowel edges to the abdominal wall skin. A loop ostomy is typically for a diverting temporary stoma (one you are going to reconnect and just temporarily divert the stool away). It is formed by bringing an intact loop of bowel through the skin opening. A cut is made approximately half way around the bowel on the exposed loop, and both the proximal and distal (upstream and downstream) ends of the loop are rolled back and sutured to the abdominal wall skin. Thus, a loop ostomy has two intestinal openings joined close to each other. A loop ostomy may appear larger than an end ostomy because of the two openings. This may make fitting an appropriate appliance for a loop ostomy slightly more challenging.
Loop ileostomy: ASCRS Photo Gallery
Although there are many similarities among the different types of ostomies, there also are important differences that would affect how the ostomy functions. Your colorectal surgeon can answer questions about which part of the bowel the ostomy is made of, whether the ostomy is intended to be temporary or permanent, and whether it is an end or a loop ostomy. A wound ostomy continence nurse (WOC nurse or enterostomal therapist) is a registered nurse who has additional education and training in how to care for patients who have an ostomy, and may assist your colorectal surgeon in helping you plan, care and live with your ostomy.
HOW DOES AN OSTOMY IMPACT MY BOWEL MOVEMENTS?
Once your ostomy is created, your bowel movements will naturally empty through the stoma. An ostomy appliance is a plastic pouch, held to the skin around your ostomy with an adhesive skin barrier. The appliance is designed to provide secure and odor-free control of bowel movements, by collecting the stool and gas that are eliminated from your ostomy. The pouch is made of waterproof plastic, is odor-free, and is sealed. The pouch is disposable and is emptied or changed as needed. The adhesive sticks to the skin around the stoma and protects the skin from moisture or stool contents.
It is important to keep the skin around the ostomy as healthy as the skin elsewhere by wearing an ostomy appliance that fits well and stays in place. Each time you remove your skin barrier and pouch; look carefully at the skin for any swelling, redness, rash or other signs of irritation. Ostomy appliance systems are quite secure; "accidents" are not common. Your colorectal surgeon and WOC nurse will teach you how to attach and care for an ostomy appliance.
The frequency and quantity of your bowel movements that empty through the ostomy will vary, depending on the type of ostomy you have, your diet, and your bowel habits prior to surgery. You are encouraged to try and establish a routine for changing your pouch as soon as possible. You may need to empty your ostomy bag several times per day, but will likely only need to completely remove the ostomy appliance from your skin two to three times per week.
Early after surgery, the stool from an ileostomy is generally a liquid type of drainage. However, as the small intestine begins to adapt, the stool will become thicker and more paste-like. On the other hand, the stool from a colostomy is generally pasty and semi-formed.
WHERE WILL THE OSTOMY BE PLACED?
Before surgery, it is best for your colorectal surgeon or WOC nurse to mark an appropriate place on your abdominal wall for the ostomy and assess any special circumstances you may have that would favor one potential stoma location over another. An ostomy is best placed on a flat portion of the abdominal wall that can be easily seen and reached by you. The marking is usually done with the patient in sitting, standing and lying positions. Attention is given to skin creases, skin folds, scars, belt line, pant height, and abdominal shape. The ostomy is placed through the muscles that run up and down just to the left or right of the midline in your abdomen. A colostomy is usually placed to the left of your navel and an ileostomy to the right.
HOW WILL AN OSTOMY AFFECT THE ACTIVITIES OF MY DAILY LIVING?
Having any type of surgery can affect how you look and feel about your body, including your ostomy. Adjusting to your body after surgery may take some time. It is important to stay positive, learn to adapt, and get back to living. Your colorectal surgeon and your WOC nurse will support you through this time of adjustment with practical tips so you can maintain a healthy and happy life.
Below we discuss how having an ostomy impacts some of the common activities of daily living:
WILL MY DIET BE LIMITED?
Many patients can eat a regular diet with little restrictions. Depending on the type of your ostomy, you may be instructed to modify your eating habits in order to control the frequency and consistency of your bowel movements. The average daily output of an ileostomy is about 500 ml per day, but may be up to 1,000-1,500 mls in a day. The average daily output of a colostomy is about 500 ml per day, with a range of about 200-700ml.
You should learn to monitor the amount and consistency of your bowel movements. Outputs consistently above average levels may put patients at risk for dehydration; a sudden drop in output associated with abdominal pain may indicate constipation or blockage. Chew your food well and drink plenty of fluids. Your colorectal surgeon, your WOC nurse, or your nutritionist/dietitian may give you practical examples of foods that may help thicken your stool, or high roughage foods that may be best avoided (to avoid potential blockages). Unless patients have had significant portions of the small intestine removed, an ostomy does not by itself cause malnutrition. Finally, over time, your ostomy will adapt, and you will learn how different foods affect your ostomy output. Most patients are able to introduce foods back into their diet a little at a time and monitor the effect of each food on the ostomy function.
WILL THE OSTOMY LIMIT MY BATHING AND MY CLOTHING?
With an ostomy, you can shower or bathe just as you did before. Soap and water will not flow into your stoma or hurt it in any way. You may shower or bathe with your pouch on or off – the choice is yours. Soap residue can sometimes interfere with how well the adhesive sticks to your skin.
While many patients worry that the pouch will be visible under their clothing, an ostomy is easily hidden by usual clothing. The ostomy appliance pouches are low profile and fit close to the body. The pouch can be worn inside or outside your underwear, whichever is more comfortable.
WILL MY PHYSICAL ACTIVITIES BE LIMITED?
An ostomy should not prevent you from exercising or enjoying the same types of physical activities as before surgery, except in cases of extremely rough contact sports or very heavy lifting. Once healing from surgery is complete, activities may be gradually resumed. If there is worry that running, swimming, or other vigorous activity may loosen the ostomy bag, a special belt or binder can be used to hold the ostomy bag in place. Occasionally, heat and moisture can affect the skin adhesive and you may need to change the appliance system more frequently. Many public figures, prominent entertainers, and even professional athletes have ostomies that do not significantly limit their activities.
WILL MY WORK AND TRAVELLING BE LIMITED?
Once you’ve recovered from surgery, your ostomy should not limit your return to work or travel. You will need to plan ahead and have extra ostomy supplies with you. You may consider planning out your first day back at work or your first trip with the help of your colorectal surgeon, your WOC nurse, and/or other ostomy patients, who may be able to provide you with some practical tips. Many medical supply stores around the world carry ostomy supplies.
WILL MY SEXUAL INTIMACY BE LIMITED?
Supportive personal relationships can be major sources of healing after any type of surgery. Most patients with ostomies resume their usual sexual activity, and normal sexual activity will not hurt the ostomy. However, because an ostomy alters the body image, some patients worry about sex and intimacy, and about acceptance by their sexual partner. Both partners will need to adjust in order to overcome this change in body image. Time, patience, understanding, and strong communication will help. Some patients may feel more confident using an opaque pouch or a pouch cover, while others may prefer different sexual positions.
Talk to your colorectal surgeon and your WOC nurse about concerns about emotional adjustment, pregnancy, and other concerns. Many support groups are also available.
WILL OTHER PEOPLE KNOW THAT I HAVE AN OSTOMY?
It's up to you to decide whom to tell about your ostomy. Some patients find that explaining the ostomy to people closest to them is a healthy way to cope with emotions. Others may limit who will need to know about the ostomy for practical purposes, and about what to say when questions from others arise. Chances are that you have been among people with ostomies and did not even know it.
WHAT ARE THE COMPLICATIONS OF AN OSTOMY?
Complications with an ostomy can occur. The most common ostomy-related problem is local skin irritation from the stoma or from the stoma appliance. These are typically minor and can be easily remedied by careful local care. Your colorectal surgeon and your WOC nurse may advise the use of different ostomy appliances, skin barriers, or other adhesives or sealants.
Dehydration and electrolyte imbalance may occur if there is diarrhea, or loose watery stool output that is high in volume. Electrolytes are minerals in your body that have an electric charge. Maintaining the right balance of electrolytes helps your body’s blood chemistry. Signs of dehydration can be subtle and range from dry mouth, reduced and dark urine, nausea, weakness, muscle cramps and feeling weak. Foods high in sugar, salt or fat should be avoided, because they can increase ostomy output. You should replenish your body by drinking plenty of fluids, including some sports drinks with balanced electrolytes. In more extreme cases, patients may need to be hospitalized and given intravenous fluids.
Intestinal obstruction or bowel blockage can occur after any abdominal surgery. Signs of blockage may include abdominal pain, cramps, sudden decrease in output, or clear watery output. Food blockage can occur when high roughage foods that had been poorly chewed or digested form a clump that causes blockage. While most often obstruction resolves with supportive care and bowel rest, it is important that you contact your colorectal surgeon and your WOC nurse if you have these symptoms.
Most patients experience only minor problems such as skin irritation and difficulty with appliance fitting. Over time from weakening of the abdominal wall around the ostomy, the hole made in the abdominal wall can stretch out, allowing other contents from inside the abdomen to bulge out alongside the ostomy. Stoma prolapse where a segment of the bowel protrudes out of the stoma can occur. It can be managed with good local care but occasionally requires surgery, if significant symptoms are not present. Finally, significant changes in body shape, such as weight loss or gain, can affect the function of an ostomy.
CONCLUSION
This material has been provided to help you understand and manage your ostomy. Living with an ostomy will require some adjustments and learning, but you can expect to enjoy a healthy and fulfilling life with your ostomy. Being well prepared can help you make your ostomy just a part of life, so that you can fully enjoying your life. Your colorectal surgeon and WOC nurse will provide you with skills and support to help you adjust to and live with your ostomy.
WHAT IS A COLON AND RECTAL SURGEON?
Colon and rectal surgeons are experts in the surgical and non-surgical treatment of the colon, rectum and anus. They have completed advanced training in the treatment of these diseases as well as full general surgical training. Board-certified colon and rectal surgeons complete residencies in general surgery and colon and rectal surgery, and pass intensive examinations conducted by the American Board of Surgery and the American Board of Colon and Rectal Surgery. They are well-versed in the treatment of both benign and malignant diseases of the colon, rectum and anus and are able to perform routine screening examinations and surgically treat conditions if indicated to do so.
DISCLAIMER
The American Society of Colon and Rectal Surgeons is dedicated to ensuring high-quality patient care by advancing the science, prevention and management of disorders and diseases of the colon, rectum and anus. These brochures are inclusive but not prescriptive. Their purpose is to provide information on diseases and processes, rather than dictate a specific form of treatment. They are intended for the use of all practitioners, health care workers and patients who desire information about the management of the conditions addressed. It should be recognized that these brochures should not be deemed inclusive of all proper methods of care or exclusive of methods of care reasonably directed to obtain the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances
presented by the individual patient.
CITATIONS AND ADDITIONAL SOURCES OF INFORMATION
Sands, L. and Marchetti, F. Chapter 31. Intestinal Stomas. Chapter in Beck, D.E., Roberts, P.L., Saclarides, T.J., Senagore, A.J., Stamos, M.J., Wexner, S.D., Eds. ASCRS Textbook of Colon and Rectal Surgery, 2nd Edition. Springer, New York, NY: 2011.
Surgical Patient Education, Ostomy Home Skills, Program website, https://www.facs.org/education/patient-education/skills-programs/ostomy-program
The United Ostomy Associations of America website, http://www.ostomy.org
The Wound, Ostomy and Continence Nurses Society website: www.wocn.org