WHAT IS AN ANAL FISSURE?
An anal fissure is a small tear in skin that lines the opening of the anus. Fissures typically cause severe pain and bleeding with bowel movements. Fissures are quite common in the general population, but are often confused with other causes of pain and bleeding, such as hemorrhoids.
Anal fissures can occur at any age and have equal gender distribution. 85-90% fissures occur in the posterior midline (back) of the anus with about 10-15% occurring in the anterior midline (front). A small number of patients may actually have fissures in both the front and the back locations. Fissures located elsewhere (off to the side) should raise suspicion for other diseases (see below) and will need to be examined further.
WHAT ARE THE SYMPTOMS OF AN ANAL FISSURE?
The typical symptoms of an anal fissure include pain and bleeding with bowel movements. Patients note severe pain during, and especially after a bowel movement, lasting from several minutes to a few hours. Patients often notice bright red blood from the anus that can be seen on the toilet paper or on the stool. Between bowel movements, patients with anal fissures are often relatively symptom-free. Many patients are fearful of having a bowel movement and may try to avoid defecation secondary to the pain.
WHAT CAUSES AN ANAL FISSURE?
Fissures are usually caused by trauma to the inner lining of the anus. A hard, dry bowel movement is typically responsible, but loose stools and diarrhea can also be the cause. The injury to the tissue creates severe anal pain, resulting in anal sphincter spasm and a subsequent increase in anal sphincter muscle pressure. The increase in anal sphincter muscle pressure results in a decrease in blood flow to the site of the injury, thus impairing healing of the wound. Ensuing bowel movements result in more pain, more anal spasm, diminished blood flow to the area, and the cycle is propagated. Treatment strategies are aimed at interrupting this cycle to promote healing of the fissure.
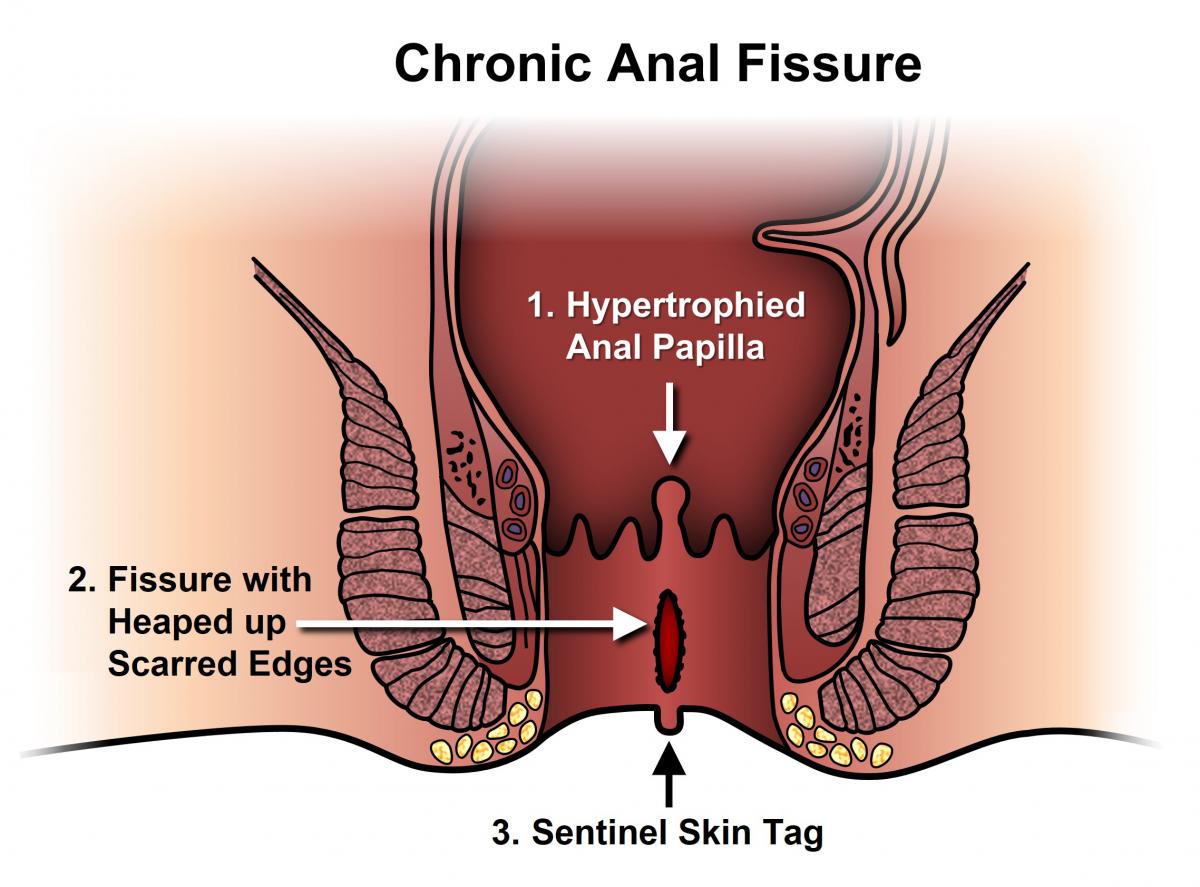
Anal fissures may be acute (recent onset) or chronic (typically lasting more than 8-12 weeks). Acute fissures may have the appearance of a simple tear in the anus, whereas chronic fissures may have swelling and scar tissue present. Chronic fissures may be more difficult to treat and may also have an external lump associated with the tear, called a sentinel pile or skin tag, as well as extra tissue just inside the anal canal, referred to as a hypertrophied papilla.
Quite commonly, anal fissures are misdiagnosed as hemorrhoids by the patient or the primary care physician due to some similar symptoms between the two. This delay in diagnosis may lead to an acute fissure becoming a chronic one and, thus, becomes more difficult to treat. Misdiagnosis of an anal fissure may also allow other conditions to go undetected and untreated, such as serious infections or even cancer. Less common causes of fissures include inflammatory conditions and certain anal infections or tumors, such as Crohn’s disease, Ulcerative Colitis, syphilis, tuberculosis, leukemia, HIV/AIDS, or anal cancer. These diseases can cause atypical fissures that are located off the midline, are multiple, painless, or non-healing after proper treatment.
WHAT IS THE TREATMENT OF ANAL FISSURES?
The majority of anal fissures do not require surgery. The most common treatment for an acute anal fissure consists of making one’s stool more consistent with a diet high in fiber as well as utilizing over-the-counter fiber supplementation (totaling 25-35 grams of fiber/day). Stool softeners and increasing water intake may be necessary to promote soft bowel movements and aid in the healing process. Antidiarrheals may be needed for loose, frequent stools. Topical anesthetics, such as lidocaine, can be used for anal pain and warm tub baths (sitz baths) for 10-20 minutes several times a day (especially after bowel movements) are soothing and promote relaxation of the anal muscles, helping the healing process.
Narcotic pain medications are not recommended for anal fissures, as they promote constipation. These non-operative measures will help achieve resolution of pain and bleeding and, potentially, heal greater than half of acute fissures with virtually no side effects. Other medications may be prescribed, when a patient has a more chronic-type fissure, that promote relaxation of the anal sphincter muscles. Your surgeon will go over benefits and side-effects of each of these with you. Chronic fissures are generally more difficult to treat, and your surgeon may advise surgical treatment either as an initial treatment or following attempts at medical management.
MEDICATIONS THAT MAY BE PRESCRIBED TO TREAT ANAL FISSURES:
Nitroglycerin Ointment
Nitroglycerin is a commonly prescribed medication that is compounded with petroleum ointment to help treat both acute and chronic anal fissures. Nitroglycerin works by chemically relaxing the internal anal sphincter muscle, which decreases sphincter pressure and subsequently increases blood flow to the injury site, resulting in healing of the fissure. Healing occurs in at least 50% of chronic fissures and the ointment can be used with the above mentioned non-operative measures, such as increasing fiber and water intake. The major side effect of nitroglycerin is headaches, which is reported in at least 20-30% of patients. Patients must also be cautioned that a drop in their blood pressure may occur, especially if other anti-hypertensive medications are being taken. Nitroglycerin can be used for variable lengths of time and can be utilized again if sustained healing is not achieved. Recurrence rates are higher with nitroglycerin than with surgery, but side effects are fewer.
Calcium Channel Blockers
These medications include diltiazem and nifedipine. Both work in a fashion similar to nitroglycerin ointment and have been associated with healing of chronic anal fissures in 65% to 95% of patients. Side effects are similar to nitroglycerin in regards to dropping of one’s blood pressure, but headaches are reported to be less, with up to 25% of patients. Oral forms of calcium channel blockers are also available, but these generally result in less fissure healing and more side effects than topical treatment.
WILL THE PROBLEM RETURN?
Fissures can recur easily, and it is quite common for a fully healed fissure to recur after a hard bowel movement or other injury. Even when the pain and bleeding have subsided, it is very important to continue good bowel habits and a diet high in fiber as a sustained lifestyle change. If the problem returns without an obvious cause, further assessment may be warranted.
WHAT CAN BE DONE IF THE FISSURE DOES NOT HEAL?
A fissure that fails to respond to conservative measures should be re-examined. Persistent hard or loose bowel movements, scarring, or spasm of the internal anal muscle all contribute to delayed healing. Other medical problems such as inflammatory bowel disease (Crohn’s disease), infections, or anal tumors can cause symptoms similar to anal fissures. Patients suffering from persistent anal pain should be examined to exclude these diseases. This may include a colonoscopy and an exam in the operating room under anesthesia with biopsies and tissue cultures.
WHAT DOES SURGERY FOR ANAL FISSURE INVOLVE?
Surgical options for treating anal fissure include Botulinum toxin (Botox®) injection into the anal sphincter and surgical division of a portion of the internal anal sphincter (lateral internal sphincterotomy). Both of these are performed typically as outpatient procedures. The goal of these surgical options is to promote relaxation of the anal sphincter, thereby decreasing anal pain and spasm, allowing the fissure to heal.
All surgical procedures carry some risk and both Botox® injection and sphincterotomy can rarely interfere with one’s ability to control gas and stool. Your colon and rectal surgeon will discuss these risks with you to determine the appropriate treatment for your particular situation.
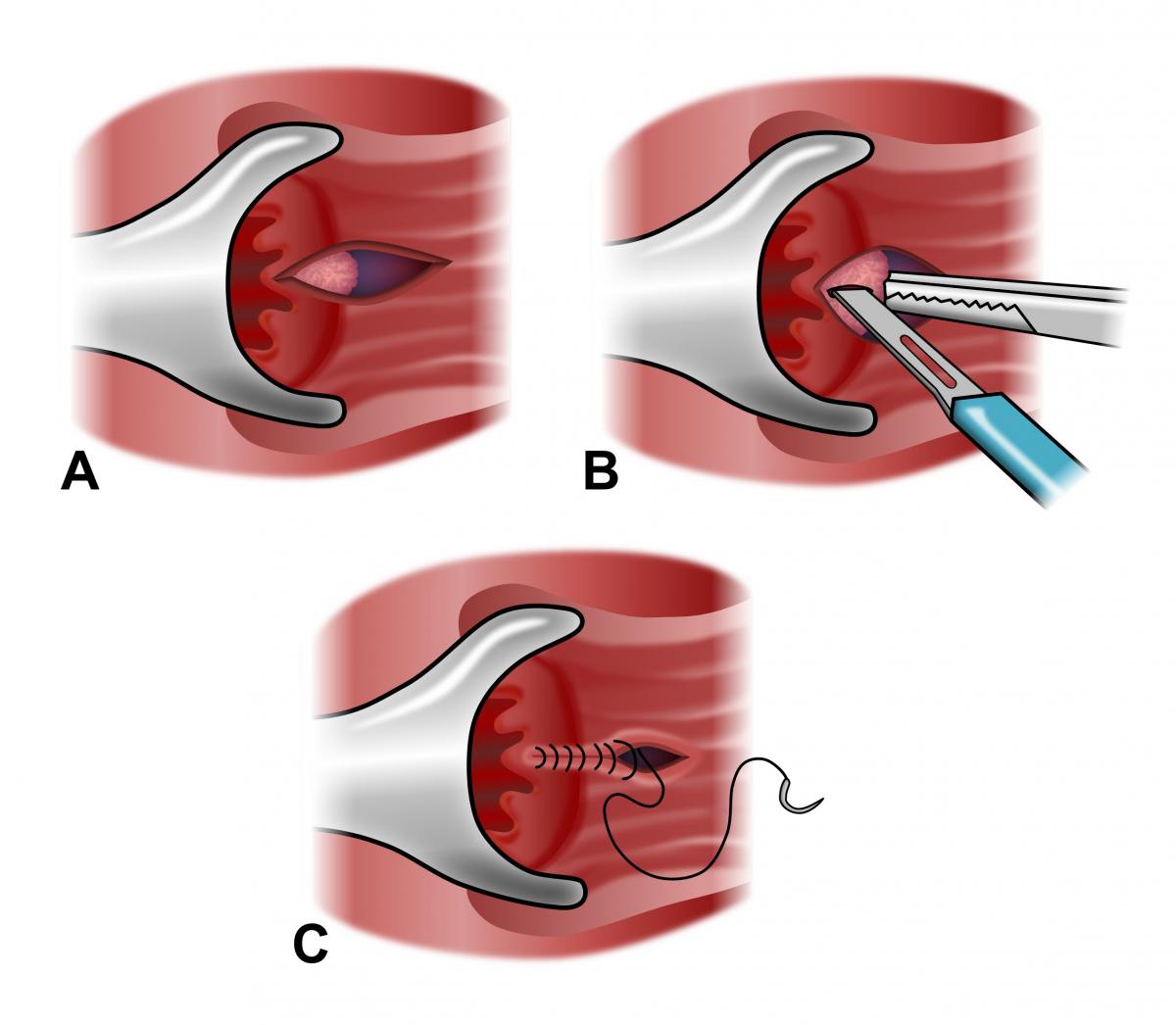
Special consideration is given to patients with established fecal incontinence, known anal sphincter muscle injury (such as after obstetric injury) or diarrheal conditions (i.e., Crohn’s disease). In these select patients, surgical sphincterotomy must be considered carefully. A thorough discussion with your surgeon will identify any of these risk factors so the most appropriate treatment can be provided. Some patients may benefit from an alternative surgery called an anal advancement flap (anoplasty). Your surgeon will discuss this with you if this option is indicated.
BOTULINUM TOXIN (BOTOX®) INJECTION
Botulinum toxin is injected directly into the internal anal sphincter muscle to promote anal sphincter relaxation and subsequent healing. This injection results in full healing in approximately 50-80% of patients. Injections are performed as an outpatient, same-day surgery procedure and, occasionally, can be performed in the office setting. Recurrences may occur in up to 40% of patients, but patients may be re-injected with good rates of fissure healing. Patients in whom Botulinum toxin injection fail are often recommended for traditional surgical sphincterotomy.
LATERAL INTERNAL SPHINCTEROTOMY
Precise and controlled division of the internal anal sphincter muscle is a highly effective and commonly used method to treat chronic and refractory anal fissures, with success rates reported to be over 90%. Recurrence rates after sphincterotomy are exceedingly low when properly performed by a surgeon. The surgery is performed as an outpatient, same-day procedure. The main risks of internal sphincterotomy are variable degrees of stool or gas incontinence. If any incontinence is present after surgery, it may resolve over a short time period. Patients undergoing sphincterotomy have much improved quality of life as compared to patients with persistent anal fissures. Your colon and rectal surgeon will go over each of the potential risks and benefits of sphincterotomy and will decide if this procedure is right for you.
HOW LONG IS THE RECOVERY AFTER SURGERY?
It is important to note that complete healing with both medical and surgical treatments can take up to approximately 6-12 weeks. However, acute pain after surgery often disappears after a few days. Most patients will be able to return to work and resume daily activities a few short days after the surgery.
CAN FISSURES LEAD TO COLON CANCER?
Absolutely not. Persistent symptoms, however, need careful evaluation since conditions other than an anal fissure can cause similar symptoms. Your colon and rectal surgeon may request additional tests, even if your fissure has successfully healed. A colonoscopy may be required to exclude other causes of rectal bleeding.
WHAT IS A COLON AND RECTAL SURGEON?
Colon and rectal surgeons are experts in the surgical and non-surgical treatment of diseases of the colon, rectum and anus. They have completed advanced surgical training in the treatment of these diseases as well as full general surgical training. Board-certified colon and rectal surgeons complete residencies in general surgery and colon and rectal surgery, and pass intensive examinations conducted by the American Board of Surgery and the American Board of Colon and Rectal Surgery. They are well-versed in the treatment of both benign and malignant diseases of the colon, rectum and anus and are able to perform routine screening examinations and surgically treat conditions if indicated to do so.
DISCLAIMER
The American Society of Colon and Rectal Surgeons is dedicated to ensuring high-quality patient care by advancing the science, prevention and management of disorders and diseases of the colon, rectum and anus. These brochures are inclusive but not prescriptive.
Their purpose is to provide information on diseases and processes, rather than dictate a specific form of treatment. They are intended for the use of all practitioners, health care workers and patients who desire information about the management of the conditions addressed. It should be recognized that these brochures should not be deemed inclusive of all proper methods of care or exclusive of methods of care reasonably directed to obtain the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances presented by the individual patient.