Pelvic floor dysfunction is a group of disorders that change the way people have bowel movements and sometimes cause pelvic pain. These disorders can be embarrassing to discuss, may be hard to diagnosis and often have a negative effect on quality of life. This information will review the most common pelvic floor dysfunction disorders and their symptoms. It is intended to explain the tests used to evaluate the pelvic floor and the various treatment options. A thorough, stepwise approach to evaluate symptoms typically leads to a prompt diagnosis and treatment for what often is a long-standing and frustrating problem.
WHAT IS THE PELVIC FLOOR?
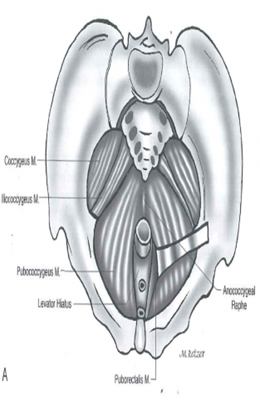
The pelvic floor is a sheet of supportive muscles through which the rectum passes and becomes the anal canal. The anal canal is surrounded by the anal sphincter complex, which is comprised of an internal and external component. Many of the disorders above are due to improper functioning of the pelvic floor muscles. The levator ani muscle is the major component of the pelvic floor and is made up of three individual muscles - the iliococygeus, pubococcygeus, and puborectalis. The puborectalis muscle is a U-shaped muscle that attaches to the pubic bone and wraps around the rectum. Under normal circumstances this muscle is contracted and creates a “bend” in the rectum, which helps to maintain stool continence. The act of bearing down to pass a bowel movement typically causes this muscle to relax, straightening out this “bend” and helping facilitate the passage of stool out of the rectum.
The urethra is the last segment of the urinary system which carries urine from the bladder to the outside. The urethra also passes through the pelvic floor in the front of the rectum. In females, the vagina also passes through the pelvic floor in between the rectum and the urethra.
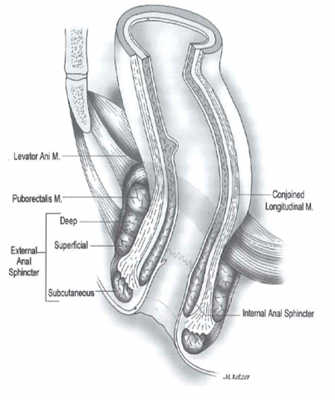
Left: The relationship of the rectum as it passes through the pelvic floor and becomes the anus, surrounded by the anal sphincter complex.
Right: A view of the pelvic floor muscles from above.
ASCRS Textbook 2nd edition, pages 11 and 3.
HOW IS PELVIC FLOOR DYSFUNCTION EVALUATED?
The most important part of evaluating a patient with suspected pelvic floor dysfunction is a personal medical history and physical examination. This includes a thorough history of the patient’s bowel patterns, urinary symptoms, any prior surgical procedures and obstetrical (childbearing) history in women. A complete physical examination is also very important and includes rectal and vaginal examinations in women.
After a complete history and physical examination, several tests may be performed. These tests can sometimes be uncomfortable or somewhat embarrassing for the patient but can provide valuable information to help determine what is causing the patient’s symptoms and help provide some relief.
ENDOANAL/ENDORECTAL ULTRASOUND:
This test provides pictures of the pelvic floor, anus, and sphincter muscles. It is performed by placing a slender ultrasound probe into the anus and/or rectum. During the test, you may be asked to squeeze or bear down, like you would do to pass a bowel movement. The test is sometimes performed in conjunction with a transvaginal ultrasound, where the ultrasound probe is placed in the vagina and/or an ultrasound of the perineum, the area of skin between the anus and vagina. Patients are usually asked to perform an enema prior to the test to empty the anus and rectum.
ANORECTAL MANOMETRY:
This test provides information regarding the strength of the anal sphincter muscles at rest and with voluntary attempts to squeeze the muscle. It also provides information about the sensation, the feeling when you must pass a bowel movement. It also provides information about the function of reflexes in the anus and rectum that are necessary to pass stool. The test involves placing a small flexible catheter (about the diameter of a pencil) with a small balloon on the end into the rectum. Like the ultrasound test, patients typically perform an enema to empty the rectum prior to the test. Patients are awake during the procedure and must be able to follow commands such as holding or passing a bowel movement and indicating when they feel certain sensations.
PUDENDAL NERVE MOTOR LATENCY TESTING:
This test evaluates the function of the pudendal nerve by measuring the amount of time between stimulation of the nerve and contraction of the sphincter muscle. It involves stimulation of the pudendal nerve from inside the anus using an electrode on the end of the examiner’s finger. The stimulation of the nerve and resulting muscle contraction may be uncomfortable for the patient.
ELECTROMYOGRAPHY (EMG):
EMG is another means of evaluating the activity of the nerves and muscles of the anal sphincter and pelvic floor. This test may be performed by using a number of small needles placed into the anal muscles or by using an anal plug with surface electrodes. This test may also be uncomfortable but can be very useful in detecting and treating patients with fecal incontinence and dyssynergic defecation.
VIDEO DEFECOGRAPHY:
This study most realistically re-creates what happens during an actual bowel movement. Before the test the patient is given an enema of thickened liquid, called contrast, that is seen on x-rays. Addition contrast material may also be given orally and vaginally. X-ray video images are then taken while the patient sits on a special commode and evacuates the contrast material as they would during a bowel movement. This test provides valuable information for patients with dyssynergic defecation and pelvic organ prolapse.

MAGNETIC RESONANCE (MR) DEFECOGRAPHY:
This test is similar to traditional video defecography, but the images are captured with the use of an MRI rather than regular x-rays. Like video defecography, contrast material is placed into the rectum and vagina and the patient is asked to bear down and simulate passing a bowel movement. The test is done within an MRI machine and the patient is positioned lying down on their back. This is a relatively new procedure that may only be performed in selected centers.
TYPES OF PELVIC FLOOR DYSFUNCTION
RECTOCELE
The vagina and the rectum can be thought of as two muscular tubes running parallel to each other and sharing a common muscular wall between them – the back wall of the vagina and the front wall of the rectum together make up what is called the “rectovaginal septum”. A rectocele occurs when the rectovaginal septum becomes weak and the rectum bulges forwards into the vagina.
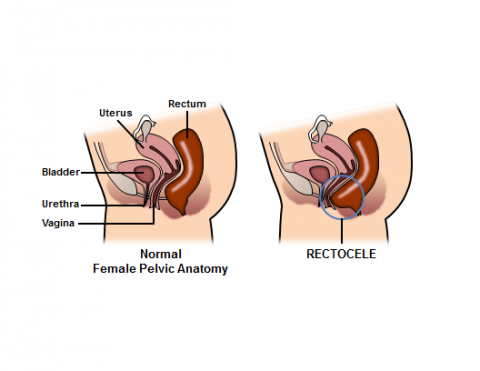
Rectocele Diagram Courtesy of Robin Noel
Hospital of the University of Pennsylvania
Department of Surgery
4th Floor Maloney Building, Fitts Education Center
Philadelphia, PA 19104
215-349-5043
www.uphs.upenn.edu/surgery/
www.uphs.upenn.edu/surgery/admin/noel.html
When a rectocele becomes large, stool can become trapped within it, making it difficult to have a bowel movement or creating a sensation of incomplete evacuation. During bowel movements, women with large, symptomatic rectoceles may describe the need to put their fingers into their vagina and push back toward the rectum to allow the stool to pass, this is called splinting.
Often a rectocele can be easily recognized on physical examination. Video or MR defecography can be useful in making the diagnosis and further evaluating a rectocele. In patients with rectoceles, these tests show contrast material bulging from the front of the rectum into the back of the vagina.
In the absence of severe symptoms, the treatment is focused on optimizing stool consistency to aid in the passage of stool. This often involves increasing fiber intake, such as taking a daily fiber supplement, and increasing fluid intake. Biofeedback, which is a special form of pelvic floor physical therapy aimed at improving a patient’s rectal sensation and pelvic floor muscle contraction, may also be helpful. As described above, the patient may insert one or two fingers into the vagina to splint the vagina during attempts to pass stool.
When symptoms persist despite appropriate non-surgical measures, surgical treatment may be considered. This usually involves reinforcement of the rectovaginal septum, either through the rectum, the perineum (space between rectum and vagina) or through the vagina.
ANISMUS (DYSSYNERGIC DEFECATION)
The process of defection is complex involving the propulsion of stool by the rectum above and the coordinated relaxation of the pelvic floor and anal sphincter muscles for stool to be evacuated. Anismus occurs when the pelvic floor and sphincter muscles do not relax when bearing down to pass stool. In some cases, these muscles contract harder, resulting in difficulty emptying the rectum. Because the puborectalis muscle of the pelvic floor may actually contract rather than relax to pass stool this condition has been known as paradoxical (non-relaxing) puborectalis syndrome. Patients often complain of the sensation of “pushing against a closed door”. The exact cause is unclear, but it is thought to be due to a combination of factors that may include improper functioning of the nerves and/or muscles of the pelvic floor.
The diagnosis is considered in patients with longstanding difficulty passing bowel movements. Various testing modalities including manometry, EMG, and defecography came help confirm the diagnosis. These tests demonstrate the inability to push stool from the rectum through the anal sphincter muscles during the evacuation of a bowel movement.
The mainstay of treatment is biofeedback therapy. As patients perform this specialized form of pelvic floor physical therapy, they are often able to view EMG or manometry tracings produced by a sensor in the rectum so that they can visualize the results of their efforts to relax the pelvic floor. Portable units have even been developed for home use. Most failures are due to the patient not keeping up with their exercises or performing them incorrectly.
PELVIC PAIN SYNDROMES
LEVATOR ANI SYNDROME
Patients with levator ani syndrome experience episodic pain, pressure, or discomfort in the rectum, pelvis, or gluteal region. The pain is often described as a vague, dull, or achy pressure sensation high in the rectum that may be worse with sitting. The pain comes and goes and may last for hours or days. The exact cause is not known, but anxiety and depression have been closely associated with levator ani syndrome.
There is no test that will definitively confirm the diagnosis of levator ani syndrome. It is often considered a “diagnosis of exclusion,” meaning that care must be taken to rule out other causes of pain before making a diagnosis of levator ani syndrome. Patients often experience similar discomfort during a digital rectal examination when the examiner’s finger places traction on the puborectalis muscle.
Several methods of treatment are available for levator ani syndrome. Physical therapy, including digital massage of the puborectalis with a combination of heat and muscle relaxants has been shown to be most effective in reducing symptoms. Injection of local anesthetics and anti-inflammatory agents into the puborectalis muscle may provide relief, though the results are often inconsistent and short-lived. Biofeedback therapy has been used with excellent results.
PROCTALGIA FUGAX
Proctalgia fugax is characterized by fleeting pain in the rectum that lasts for just a minute or two. Because the pain comes and goes quickly and unpredictably, it is difficult to evaluate. It is thought that it is probably due to spasm of the rectum and/or the muscles of the pelvic floor and may wake patients from sleep.
Proctalgia fugax may be diagnosed after a careful history and examination and thorough evaluation have been performed to rule out more serious causes of rectal pain.
Support measures should be used as needed for relief of symptoms such as change in patients’ position, reassurance, warm baths, or medications. The patient should be reassured otherwise that the symptoms are not a sign of another more serious disorder.
COCCYGODYNIA
Coccygodynia is characterized by distinct pain that is evoked with pressure or manipulation of the coccyx or tailbone. It is usually due to a history of trauma to the tailbone. Other causes include weakening of the tailbone due to poor blood flow (avascular necrosis) and referred pain from herniated lumbar disc.
It usually is diagnosed by a combination of history and physical examination. X-rays should be done to rule out either a recent or longstanding fracture of the tailbone.
Injection of local anesthetics and anti-inflammatory agents with manipulation of tailbone under anesthesia can provide relief from pain for most patients. Coccygectomy, surgical excision of the tailbone, may be considered for those who fail injection therapy.
PUDENDAL NEURALGIA
Pudendal neuralgia is caused by entrapment of the pudendal nerve by pelvic muscles and ligaments. It is characterized by chronic pain in pelvis or perineum, between the penis/clitoris to the anus, and is usually worse with sitting.
The diagnosis is suggested by history and physical examination. Relief of symptoms after a pudendal nerve block and an MRI are often helpful in making the diagnosis.
Initial management usually consists of physical therapy and anti-inflammatory agents. Other treatment options include pudendal nerve block, nerve ablation, and neuromodulation. Surgical decompression of entrapped nerves may be considered in refractory cases.
WHAT IS A COLON AND RECTAL SURGEON?
Colon and rectal surgeons are experts in the surgical and non-surgical treatment of diseases of the colon, rectum, and anus. They have completed advanced surgical training in the treatment of these diseases, as well as full general surgical training. They are well versed in the treatment of both benign and malignant diseases of the colon, rectum and anus and are able to perform routine screening examinations and surgically treat conditions, if indicated to do so.
DISCLAIMER
The American Society of Colon and Rectal Surgeons is dedicated to ensuring high-quality patient care by advancing the science, prevention and management of disorders and diseases of the colon, rectum and anus. These brochures are inclusive but not prescriptive. Their purpose is to provide information on diseases and processes, rather than dictate a specific form of treatment. They are intended for the use of all practitioners, health care workers and patients who desire information about the management of the conditions addressed. It should be recognized that these brochures should not be deemed inclusive of all proper methods of care or exclusive of methods of care reasonably directed to obtain the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances presented by the individual patient.
REFERENCES:
Harford, F.J., Brubaker, L. “Pelvic Floor Disorders.” Chapter 49 in Wolff, B. G., Fleshman, J. W., Beck, D. E., Pemberton, J.H., Wexner, S. D., Eds. The ASCRS Textbook of Colon and Rectal Surgery. Springer, New York, NY, 2007.
Timmcke, A. “Functional Anorectal Disorders.” Chapter 7 in Beck, D. E., Wexner, S. D., Eds. Fundamentals of Anorectal Surgery, 2nd Edition. WB Saunders, London, England, 2002.
Green, S. E., Oliver, G. C. “Proctalgia Fugax, Levator Syndrome, and Pelvic Pain.” Chapter 18 in Beck, D. E., Wexner, S. D., Eds. Fundamentals of Anorectal Surgery, 2nd Edition. WB Saunders, London, England, 2002.
Thorsen, Amy J, and Leslie Roth. "Common Tests for the Pelvic Floor." ASCRS Textbook of Colon and Rectal Surgery, 2022. ASCRS U, www.ascrsu.com/ascrs/view/ASCRS-Textbook-of-Colon-and-Rectal-Surgery/2285053/all/Common_Tests_for_the_Pelvic_Floor.
Kunitake, Hiroko, and Kyle Staller. "Functional Disorders After Colorectal Surgery/IBS." ASCRS Textbook of Colon and Rectal Surgery, 2022. ASCRS U, www.ascrsu.com/ascrs/view/ASCRS-Textbook-of-Colon-and-Rectal-Surgery/2285052/all/Functional_Disorders_After_Colorectal_Surgery_IBS.
Zutshi, Massarat, and Lucia C Castro Oliveira. "Treatment of Difficult/Obstructive Defecation." ASCRS Textbook of Colon and Rectal Surgery, 2022. ASCRS U, www.ascrsu.com/ascrs/view/ASCRS-Textbook-of-Colon-and-Rectal-Surgery/2285055/all/Treatment_of_Difficult_Obstructive_Defecation.